Small tile blue
maxgraft® granules
For experienced oral and maxillofacial surgeons, allograft bone is the only real alternative to harvesting the patient’s own autologous bone. This helps preventing well known risks such as donor-site morbidity, infection, post-operative pain, and bone-stability loss. The excellent biological regeneration capability of maxgraft® results in a predictable clinical outcome.
|
Rehydration
The processing of maxgraft® products preserves the natural collagen content and a residual water content of <10%. Thus, a rehydration is not mandatory. However, rehydration in blood or saline solution can facilitate the handling and application of maxgraft® granules due to better sticking together.
Rehydration
The processing of maxgraft® products preserves the natural collagen content and a residual water content of <10%. Thus, a rehydration is not mandatory. However, rehydration in blood or saline solution can facilitate the handling and application of maxgraft® granules due to better sticking together.
Rehydration
The processing of maxgraft® products preserves the natural collagen content and a residual water content of <10%. Thus, a rehydration is not mandatory. However, rehydration in blood or saline solution can facilitate the handling and application of maxgraft® granules due to better sticking together.
Rehydration
The processing of maxgraft® products preserves the natural collagen content and a residual water content of <10%. Thus, a rehydration is not mandatory. However, rehydration in blood or saline solution can facilitate the handling and application of maxgraft® granules due to better sticking together.
Rehydration
The processing of maxgraft® products preserves the natural collagen content and a residual water content of <10%. Thus, a rehydration is not mandatory. However, rehydration in blood or saline solution can facilitate the handling and application of maxgraft® granules due to better sticking together.
Rehydration
The processing of maxgraft® products preserves the natural collagen content and a residual water content of <10%. Thus, a rehydration is not mandatory. However, rehydration in blood or saline solution can facilitate the handling and application of maxgraft® granules due to better sticking together.
Particle application
Avoid compressing the particles excessively during application; less packed particles leave more space for blood vessel ingrowth and formation of new bone matrix.
Particle application
Avoid compressing the particles excessively during application; less packed particles leave more space for blood vessel ingrowth and formation of new bone matrix.
Particle application
Avoid compressing the particles excessively during application; less packed particles leave more space for blood vessel ingrowth and formation of new bone matrix.
Particle application
Avoid compressing the particles excessively during application; less packed particles leave more space for blood vessel ingrowth and formation of new bone matrix.
Particle application
Avoid compressing the particles excessively during application; less packed particles leave more space for blood vessel ingrowth and formation of new bone matrix.
Particle application
Avoid compressing the particles excessively during application; less packed particles leave more space for blood vessel ingrowth and formation of new bone matrix.
Mixing with autologous bone
Mixing of maxgraft® granules with autologous bone adds a biological activity (osteoinductive and osteogenetic properties of autologous bone) and supports faster regeneration and formation of new bone.
Mixing with autologous bone
Mixing of maxgraft® granules with autologous bone adds a biological activity (osteoinductive and osteogenetic properties of autologous bone) and supports faster regeneration and formation of new bone.
Mixing with autologous bone
Mixing of maxgraft® granules with autologous bone adds a biological activity (osteoinductive and osteogenetic properties of autologous bone) and supports faster regeneration and formation of new bone.
Mixing with autologous bone
Mixing of maxgraft® granules with autologous bone adds a biological activity (osteoinductive and osteogenetic properties of autologous bone) and supports faster regeneration and formation of new bone.
Mixing with autologous bone
Mixing of maxgraft® granules with autologous bone adds a biological activity (osteoinductive and osteogenetic properties of autologous bone) and supports faster regeneration and formation of new bone.
Mixing with autologous bone
Mixing of maxgraft® granules with autologous bone adds a biological activity (osteoinductive and osteogenetic properties of autologous bone) and supports faster regeneration and formation of new bone.
Mixing with cerabone®
Mixing of maxgraft® granules with xenogenic materials (cerabone®) combines the advantages of both materials; the biological potential of maxgraft® and the long-term volume stability of cerabone® lead to fast regeneration of strong vital bone.
Mixing with cerabone®
Mixing of maxgraft® granules with xenogenic materials (cerabone®) combines the advantages of both materials; the biological potential of maxgraft® and the long-term volume stability of cerabone® lead to fast regeneration of strong vital bone.
Mixing with cerabone®
Mixing of maxgraft® granules with xenogenic materials (cerabone®) combines the advantages of both materials; the biological potential of maxgraft® and the long-term volume stability of cerabone® lead to fast regeneration of strong vital bone.
Mixing with cerabone®
Mixing of maxgraft® granules with xenogenic materials (cerabone®) combines the advantages of both materials; the biological potential of maxgraft® and the long-term volume stability of cerabone® lead to fast regeneration of strong vital bone.
Mixing with cerabone®
Mixing of maxgraft® granules with xenogenic materials (cerabone®) combines the advantages of both materials; the biological potential of maxgraft® and the long-term volume stability of cerabone® lead to fast regeneration of strong vital bone.
Mixing with cerabone®
Mixing of maxgraft® granules with xenogenic materials (cerabone®) combines the advantages of both materials; the biological potential of maxgraft® and the long-term volume stability of cerabone® lead to fast regeneration of strong vital bone.
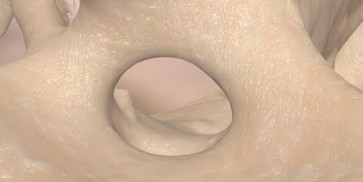
Re-entry
Depending on the defect size, the graft will be incorporated stable within 3-4 months (usage of maxgraft® granules in socket preservation, smaller bone defects, periodontal defects).
Re-entry
Depending on the defect size, the graft will be incorporated stable within 3-4 months (usage of maxgraft® granules in socket preservation, smaller bone defects, periodontal defects).
Re-entry
Depending on the defect size, the graft will be incorporated stable within 3-4 months (usage of maxgraft® granules in socket preservation, smaller bone defects, periodontal defects).
Re-entry
Depending on the defect size, the graft will be incorporated stable within 3-4 months (usage of maxgraft® granules in socket preservation, smaller bone defects, periodontal defects).
Re-entry
Depending on the defect size, the graft will be incorporated stable within 3-4 months (usage of maxgraft® granules in socket preservation, smaller bone defects, periodontal defects).
Re-entry
Depending on the defect size, the graft will be incorporated stable within 3-4 months (usage of maxgraft® granules in socket preservation, smaller bone defects, periodontal defects).
maxgraft® blocks
For experienced oral and maxillofacial surgeons, allograft bone blocks for block augmentation are the only real alternative to harvesting the patient’s own autologous bone. This helps preventing well known risks such as donor-site morbidity, infection, post-operative pain, and bone-stability loss. The excellent biological regeneration capability of maxgraft® results in a predictable clinical outcome.
|
Contact to local bone
Avoid larger gaps between graft and defect, because a close contact between transplant and local bone ensures block incorporation and faster regeneration.
Contact to local bone
Avoid larger gaps between graft and defect, because a close contact between transplant and local bone ensures block incorporation and faster regeneration.
Contact to local bone
Avoid larger gaps between graft and defect, because a close contact between transplant and local bone ensures block incorporation and faster regeneration.
Contact to local bone
Avoid larger gaps between graft and defect, because a close contact between transplant and local bone ensures block incorporation and faster regeneration.
Contact to local bone
Avoid larger gaps between graft and defect, because a close contact between transplant and local bone ensures block incorporation and faster regeneration.
Contact to local bone
Avoid larger gaps between graft and defect, because a close contact between transplant and local bone ensures block incorporation and faster regeneration.
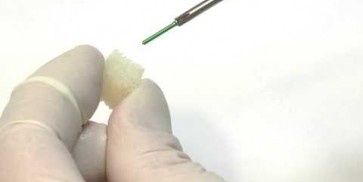
Rehydration
The processing of maxgraft® products preserves the natural collagen content and a residual water content of <10%. Thus, a rehydration is not mandatory, but it is recommended. Rehydration in saline solution results in a bit more flexibility of the block, therefore it is less prone to crumble or break and can be more easily adapted to the defect area.
Rehydration
The processing of maxgraft® products preserves the natural collagen content and a residual water content of <10%. Thus, a rehydration is not mandatory, but it is recommended. Rehydration in saline solution results in a bit more flexibility of the block, therefore it is less prone to crumble or break and can be more easily adapted to the defect area.
Rehydration
The processing of maxgraft® products preserves the natural collagen content and a residual water content of <10%. Thus, a rehydration is not mandatory, but it is recommended. Rehydration in saline solution results in a bit more flexibility of the block, therefore it is less prone to crumble or break and can be more easily adapted to the defect area.
Rehydration
The processing of maxgraft® products preserves the natural collagen content and a residual water content of <10%. Thus, a rehydration is not mandatory, but it is recommended. Rehydration in saline solution results in a bit more flexibility of the block, therefore it is less prone to crumble or break and can be more easily adapted to the defect area.
Rehydration
The processing of maxgraft® products preserves the natural collagen content and a residual water content of <10%. Thus, a rehydration is not mandatory, but it is recommended. Rehydration in saline solution results in a bit more flexibility of the block, therefore it is less prone to crumble or break and can be more easily adapted to the defect area.
Rehydration
The processing of maxgraft® products preserves the natural collagen content and a residual water content of <10%. Thus, a rehydration is not mandatory, but it is recommended. Rehydration in saline solution results in a bit more flexibility of the block, therefore it is less prone to crumble or break and can be more easily adapted to the defect area.
Combination with cerabone® oder maxresorb®
Additional void volume should be filled with particulate grafting material (e.g. cerabone® or maxresorb®) to improve the esthetic outcome and to protect the soft tissue.
Combination with cerabone® oder maxresorb®
Additional void volume should be filled with particulate grafting material (e.g. cerabone® or maxresorb®) to improve the esthetic outcome and to protect the soft tissue.
Combination with cerabone® oder maxresorb®
Additional void volume should be filled with particulate grafting material (e.g. cerabone® or maxresorb®) to improve the esthetic outcome and to protect the soft tissue.
Combination with cerabone® oder maxresorb®
Additional void volume should be filled with particulate grafting material (e.g. cerabone® or maxresorb®) to improve the esthetic outcome and to protect the soft tissue.
Combination with cerabone® oder maxresorb®
Additional void volume should be filled with particulate grafting material (e.g. cerabone® or maxresorb®) to improve the esthetic outcome and to protect the soft tissue.
Combination with cerabone® oder maxresorb®
Additional void volume should be filled with particulate grafting material (e.g. cerabone® or maxresorb®) to improve the esthetic outcome and to protect the soft tissue.
Healing time
The average healing period is about 4 months for smaller defects and 6 months for larger defects.
Healing time
The average healing period is about 4 months for smaller defects and 6 months for larger defects.
Healing time
The average healing period is about 4 months for smaller defects and 6 months for larger defects.
Healing time
The average healing period is about 4 months for smaller defects and 6 months for larger defects.
Healing time
The average healing period is about 4 months for smaller defects and 6 months for larger defects.
Healing time
The average healing period is about 4 months for smaller defects and 6 months for larger defects.
Avoiding soft tissue perforation
Use flat-headed screws for fixation and avoid sharp edges that might cause a perforation of the overlying soft tissue.
Avoiding soft tissue perforation
Use flat-headed screws for fixation and avoid sharp edges that might cause a perforation of the overlying soft tissue.
Avoiding soft tissue perforation
Use flat-headed screws for fixation and avoid sharp edges that might cause a perforation of the overlying soft tissue.
Avoiding soft tissue perforation
Use flat-headed screws for fixation and avoid sharp edges that might cause a perforation of the overlying soft tissue.
Avoiding soft tissue perforation
Use flat-headed screws for fixation and avoid sharp edges that might cause a perforation of the overlying soft tissue.
Avoiding soft tissue perforation
Use flat-headed screws for fixation and avoid sharp edges that might cause a perforation of the overlying soft tissue.
Please Contact us for Literature.
Jason® membrane
Due to the unique production process, the superior properties of the native pericardium are preserved during the extensive cleaning procedure that is applied for the production of Jason® membrane. Therefore, Jason® membrane shows a natural honeycomb-like, multilayered collagen structure with an increased content of collagen type III leading to a remarkable tear resistance to and a slow degradation of Jason® membrane. This ensures a natural long barrier function, making the Jason® membrane our recommended choice particularly for large augmentative procedures.
|
Rehydration
The Jason® membrane can be applied dry or pre-hydrated in sterile saline solution or blood from the defect. The initial placement of the dry membrane with subsequent application of the graft material is particularly advantageous for lateral augmentations. After rehydration the membrane can be folded over the defect.
Rehydration
The Jason® membrane can be applied dry or pre-hydrated in sterile saline solution or blood from the defect. The initial placement of the dry membrane with subsequent application of the graft material is particularly advantageous for lateral augmentations. After rehydration the membrane can be folded over the defect.
Rehydration
The Jason® membrane can be applied dry or pre-hydrated in sterile saline solution or blood from the defect. The initial placement of the dry membrane with subsequent application of the graft material is particularly advantageous for lateral augmentations. After rehydration the membrane can be folded over the defect.
Rehydration
The Jason® membrane can be applied dry or pre-hydrated in sterile saline solution or blood from the defect. The initial placement of the dry membrane with subsequent application of the graft material is particularly advantageous for lateral augmentations. After rehydration the membrane can be folded over the defect.
Rehydration
The Jason® membrane can be applied dry or pre-hydrated in sterile saline solution or blood from the defect. The initial placement of the dry membrane with subsequent application of the graft material is particularly advantageous for lateral augmentations. After rehydration the membrane can be folded over the defect.
Rehydration
The Jason® membrane can be applied dry or pre-hydrated in sterile saline solution or blood from the defect. The initial placement of the dry membrane with subsequent application of the graft material is particularly advantageous for lateral augmentations. After rehydration the membrane can be folded over the defect.
Fixation
Jason® membrane exhibits a remarkable multi-directional tear resistance. Therefore, it can easily be pinned, sutured or even screwed without rupturing.
Fixation
Jason® membrane exhibits a remarkable multi-directional tear resistance. Therefore, it can easily be pinned, sutured or even screwed without rupturing.
Fixation
Jason® membrane exhibits a remarkable multi-directional tear resistance. Therefore, it can easily be pinned, sutured or even screwed without rupturing.
Fixation
Jason® membrane exhibits a remarkable multi-directional tear resistance. Therefore, it can easily be pinned, sutured or even screwed without rupturing.
Fixation
Jason® membrane exhibits a remarkable multi-directional tear resistance. Therefore, it can easily be pinned, sutured or even screwed without rupturing.
Fixation
Jason® membrane exhibits a remarkable multi-directional tear resistance. Therefore, it can easily be pinned, sutured or even screwed without rupturing.
Exposure
Exposure of Jason® membrane should be avoided, since fast bacterial resorption significantly reduces the barrier function of the thin Jason® membrane. In case of an unstable soft tissue situation or if you expect a wound dehiscence to occur, it is recommended to cover the membrane with a Jason® fleece (where applicable, soaked in antibiotics) to protect the healing area. In case of a dehiscence the wound usually heals without complications by formation of free granulation tissue.
Exposure
Exposure of Jason® membrane should be avoided, since fast bacterial resorption significantly reduces the barrier function of the thin Jason® membrane. In case of an unstable soft tissue situation or if you expect a wound dehiscence to occur, it is recommended to cover the membrane with a Jason® fleece (where applicable, soaked in antibiotics) to protect the healing area. In case of a dehiscence the wound usually heals without complications by formation of free granulation tissue.
Exposure
Exposure of Jason® membrane should be avoided, since fast bacterial resorption significantly reduces the barrier function of the thin Jason® membrane. In case of an unstable soft tissue situation or if you expect a wound dehiscence to occur, it is recommended to cover the membrane with a Jason® fleece (where applicable, soaked in antibiotics) to protect the healing area. In case of a dehiscence the wound usually heals without complications by formation of free granulation tissue.
Exposure
Exposure of Jason® membrane should be avoided, since fast bacterial resorption significantly reduces the barrier function of the thin Jason® membrane. In case of an unstable soft tissue situation or if you expect a wound dehiscence to occur, it is recommended to cover the membrane with a Jason® fleece (where applicable, soaked in antibiotics) to protect the healing area. In case of a dehiscence the wound usually heals without complications by formation of free granulation tissue.
Exposure
Exposure of Jason® membrane should be avoided, since fast bacterial resorption significantly reduces the barrier function of the thin Jason® membrane. In case of an unstable soft tissue situation or if you expect a wound dehiscence to occur, it is recommended to cover the membrane with a Jason® fleece (where applicable, soaked in antibiotics) to protect the healing area. In case of a dehiscence the wound usually heals without complications by formation of free granulation tissue.
Exposure
Exposure of Jason® membrane should be avoided, since fast bacterial resorption significantly reduces the barrier function of the thin Jason® membrane. In case of an unstable soft tissue situation or if you expect a wound dehiscence to occur, it is recommended to cover the membrane with a Jason® fleece (where applicable, soaked in antibiotics) to protect the healing area. In case of a dehiscence the wound usually heals without complications by formation of free granulation tissue.
Shaping
Jason® membrane can be cut to the desired shape and size with a pair of scissors - while maintaining sterility. It may be helpful to use appropriate templates for defining the required size of the membrane.
Shaping
Jason® membrane can be cut to the desired shape and size with a pair of scissors - while maintaining sterility. It may be helpful to use appropriate templates for defining the required size of the membrane.
Shaping
Jason® membrane can be cut to the desired shape and size with a pair of scissors - while maintaining sterility. It may be helpful to use appropriate templates for defining the required size of the membrane.
Shaping
Jason® membrane can be cut to the desired shape and size with a pair of scissors - while maintaining sterility. It may be helpful to use appropriate templates for defining the required size of the membrane.
Shaping
Jason® membrane can be cut to the desired shape and size with a pair of scissors - while maintaining sterility. It may be helpful to use appropriate templates for defining the required size of the membrane.
Shaping
Jason® membrane can be cut to the desired shape and size with a pair of scissors - while maintaining sterility. It may be helpful to use appropriate templates for defining the required size of the membrane.
Placement
Jason® membrane has one rough and one slightly smoother surface. The smoother, fine structured side is marked „G“ at the top right corner and should be placed towards the gingiva. The rougher side should face the bone. However, there is no problem if the membrane is placed the other way around, since the long-term barrier function of the membrane will still provide sufficient protection for the regeneration site.
Placement
Jason® membrane has one rough and one slightly smoother surface. The smoother, fine structured side is marked „G“ at the top right corner and should be placed towards the gingiva. The rougher side should face the bone. However, there is no problem if the membrane is placed the other way around, since the long-term barrier function of the membrane will still provide sufficient protection for the regeneration site.
Placement
Jason® membrane has one rough and one slightly smoother surface. The smoother, fine structured side is marked „G“ at the top right corner and should be placed towards the gingiva. The rougher side should face the bone. However, there is no problem if the membrane is placed the other way around, since the long-term barrier function of the membrane will still provide sufficient protection for the regeneration site.
Placement
Jason® membrane has one rough and one slightly smoother surface. The smoother, fine structured side is marked „G“ at the top right corner and should be placed towards the gingiva. The rougher side should face the bone. However, there is no problem if the membrane is placed the other way around, since the long-term barrier function of the membrane will still provide sufficient protection for the regeneration site.
Placement
Jason® membrane has one rough and one slightly smoother surface. The smoother, fine structured side is marked „G“ at the top right corner and should be placed towards the gingiva. The rougher side should face the bone. However, there is no problem if the membrane is placed the other way around, since the long-term barrier function of the membrane will still provide sufficient protection for the regeneration site.
Placement
Jason® membrane has one rough and one slightly smoother surface. The smoother, fine structured side is marked „G“ at the top right corner and should be placed towards the gingiva. The rougher side should face the bone. However, there is no problem if the membrane is placed the other way around, since the long-term barrier function of the membrane will still provide sufficient protection for the regeneration site.
Please Contact us for Literature.
cerabone®
The long-term success of cerabone® is based on its excellent osteoconductive properties and exceptional purity achieved by a unique 1200°C temperature treatment processing. The unique topographic and physico-chemical characteristics of cerabone® efficiently support blood clot formation and the proliferation of regenerative cells leading to predictable particle integration. Its non-resorbability, owing to its exceptional purity, provides stability of the augmented site on a long-term basis.
|
Rehydration
Rehydration in blood from the defect site or saline solution is not necessary but facilitates handling and application since the wetted cerabone® granules stick together.
Rehydration
Rehydration in blood from the defect site or saline solution is not necessary but facilitates handling and application since the wetted cerabone® granules stick together.
Rehydration
Rehydration in blood from the defect site or saline solution is not necessary but facilitates handling and application since the wetted cerabone® granules stick together.
Rehydration
Rehydration in blood from the defect site or saline solution is not necessary but facilitates handling and application since the wetted cerabone® granules stick together.
Rehydration
Rehydration in blood from the defect site or saline solution is not necessary but facilitates handling and application since the wetted cerabone® granules stick together.
Rehydration
Rehydration in blood from the defect site or saline solution is not necessary but facilitates handling and application since the wetted cerabone® granules stick together.
Particle compression
Avoid compressing the particles excessively during application; less packed particles leave space for blood vessel ingrowth and formation of new bone matrix.
Particle compression
Avoid compressing the particles excessively during application; less packed particles leave space for blood vessel ingrowth and formation of new bone matrix.
Particle compression
Avoid compressing the particles excessively during application; less packed particles leave space for blood vessel ingrowth and formation of new bone matrix.
Particle compression
Avoid compressing the particles excessively during application; less packed particles leave space for blood vessel ingrowth and formation of new bone matrix.
Particle compression
Avoid compressing the particles excessively during application; less packed particles leave space for blood vessel ingrowth and formation of new bone matrix.
Particle compression
Avoid compressing the particles excessively during application; less packed particles leave space for blood vessel ingrowth and formation of new bone matrix.
Healing time
A healing time of at least 6 months is recommended before re-entry to ensure stable integration of the particles.
Healing time
A healing time of at least 6 months is recommended before re-entry to ensure stable integration of the particles.
Healing time
A healing time of at least 6 months is recommended before re-entry to ensure stable integration of the particles.
Healing time
A healing time of at least 6 months is recommended before re-entry to ensure stable integration of the particles.
Healing time
A healing time of at least 6 months is recommended before re-entry to ensure stable integration of the particles.
Healing time
A healing time of at least 6 months is recommended before re-entry to ensure stable integration of the particles.
Mixing of material
Mixing of cerabone® with autologous bone bring about a biological activity (osteo-inductive and osteo-genetic properties of autologous bone) and supports faster regeneration and improved formation of new bone.
Mixing of material
Mixing of cerabone® with autologous bone bring about a biological activity (osteo-inductive and osteo-genetic properties of autologous bone) and supports faster regeneration and improved formation of new bone.
Mixing of material
Mixing of cerabone® with autologous bone bring about a biological activity (osteo-inductive and osteo-genetic properties of autologous bone) and supports faster regeneration and improved formation of new bone.
Mixing of material
Mixing of cerabone® with autologous bone bring about a biological activity (osteo-inductive and osteo-genetic properties of autologous bone) and supports faster regeneration and improved formation of new bone.
Mixing of material
Mixing of cerabone® with autologous bone bring about a biological activity (osteo-inductive and osteo-genetic properties of autologous bone) and supports faster regeneration and improved formation of new bone.
Mixing of material
Mixing of cerabone® with autologous bone bring about a biological activity (osteo-inductive and osteo-genetic properties of autologous bone) and supports faster regeneration and improved formation of new bone.