Guided Tissue Regeneration
|

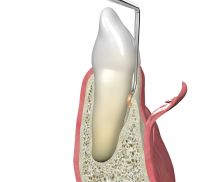
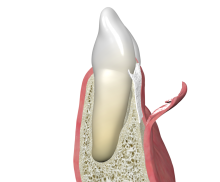
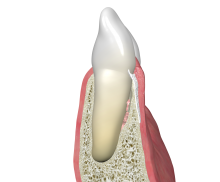
Periodontal intrabony defects can be predictably treated with a barrier membrane in the sense of GTR [4, 5]. Following flap elevation and granulation tissue removal, the root surfaces are cleaned and a membrane is placed between the gingiva and tooth to cover the defect area completely. To achieve primary wound closure, the flap is repositioned tension-free.
Collagen membranes are very widely used in GTR procedures due to inherent advantageous properties of collagen. Collagen exhibits an excellent biocompatibility and controlled, complete degradation together with a natural hemostatic activity and chemotactic attraction of fibroblasts and osteoblasts. For small bone defects like periodontal intrabony defects the collprotect® membrane with intermediate barrier function is the optimal choice. Of course, the pericardium membrane, Jason® membrane, which offers a significantly longer barrier function, may also be applied.
Non-contained intrabony defects (1- or 2-wall defects) usually require support of the soft tissue, thus different kind of bone grafts may be used. cerabone® is a natural bovine bone graft consisting of pure bone mineral. Due to its natural bone structure cerabone® provides optimal support for bone forming cells and blood vessels. A further alternative are the allogenic maxgraft® granules or the synthetic material maxresorb®. maxresorb® is a biphasic material composed of 60% hydroxyapatite and 40% beta-tricalcium phosphate. While the fast resorption of beta-TCP quickly offers space for new bone formation, the HA component provides volume stability for an extended time period.