Sinus lift two-stage with cerabone® and Jason® membrane - Prof. Dr. Dr. D. Rothamel
-
1/19 - Initial situation after root channel treatmentSinus lift two-stage with cerabone® and Jason® membrane - Prof. Dr. Dr. D. Rothamel
-
2/19 - Detail of OPGSinus lift two-stage with cerabone® and Jason® membrane - Prof. Dr. Dr. D. Rothamel
-
3/19 - OPG after tooth extraction and healing showing vertical and lateral defect after cystectomy and tooth extractionSinus lift two-stage with cerabone® and Jason® membrane - Prof. Dr. Dr. D. Rothamel
-
4/19 - Detail of OPGSinus lift two-stage with cerabone® and Jason® membrane - Prof. Dr. Dr. D. Rothamel
-
5/19 - Clinical situation before surgerySinus lift two-stage with cerabone® and Jason® membrane - Prof. Dr. Dr. D. Rothamel
-
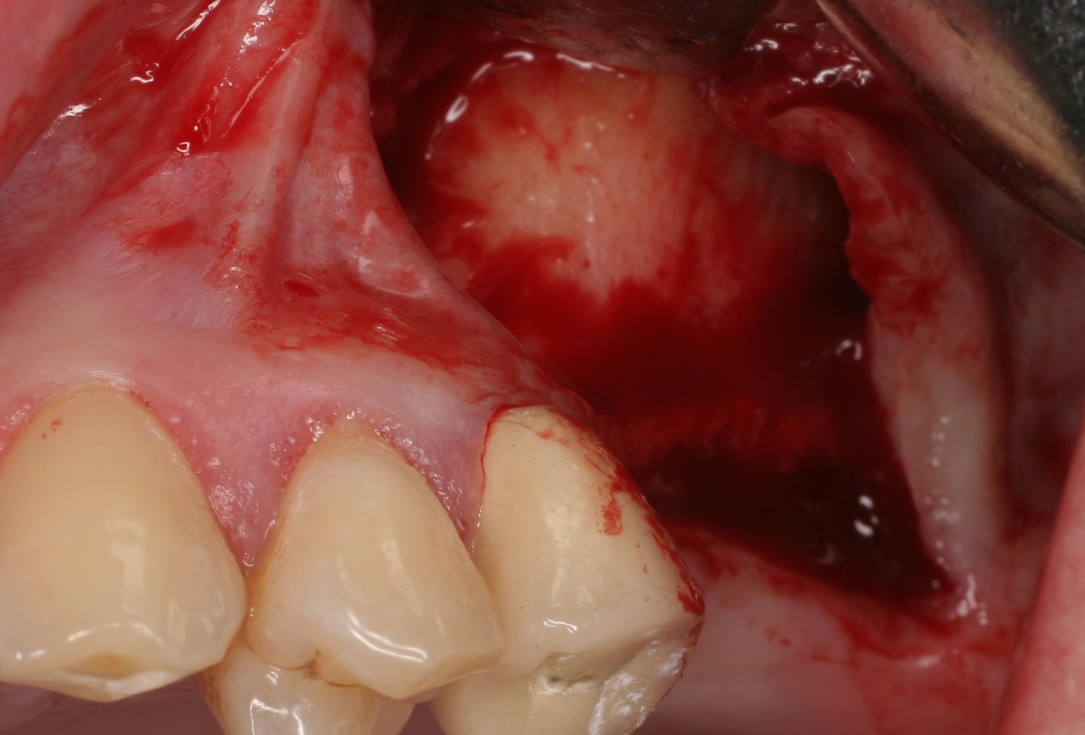
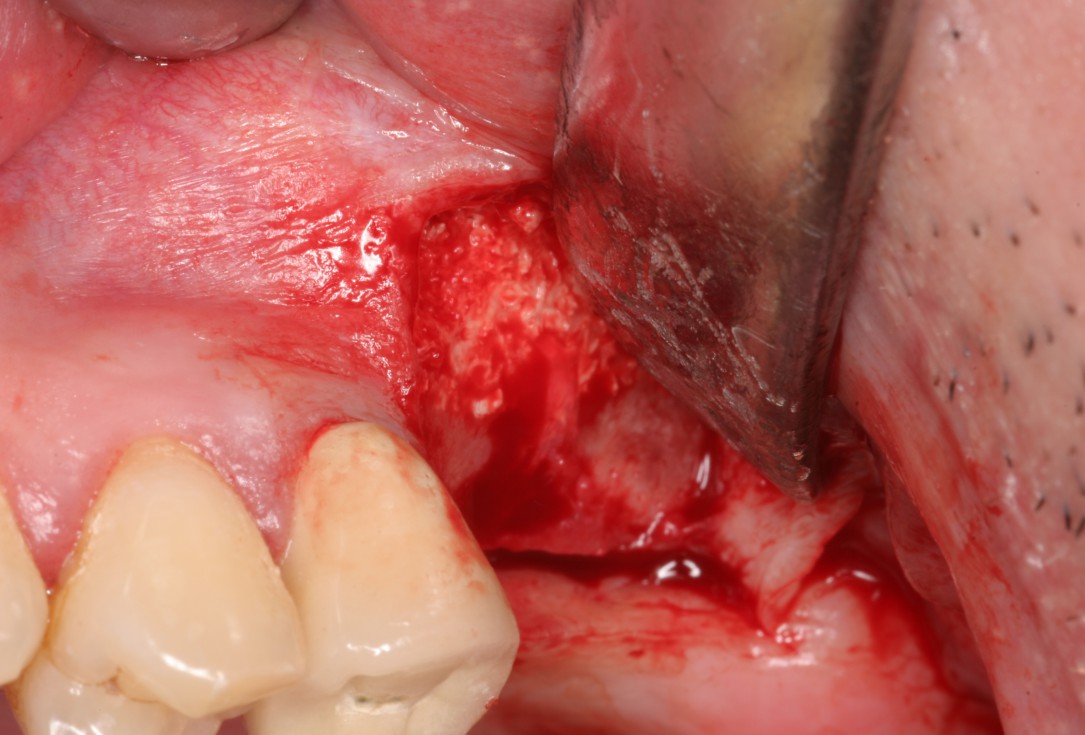
6/19 - Surgical presentation of the atrophic alveolar ridgeSinus lift two-stage with cerabone® and Jason® membrane - Prof. Dr. Dr. D. Rothamel
-
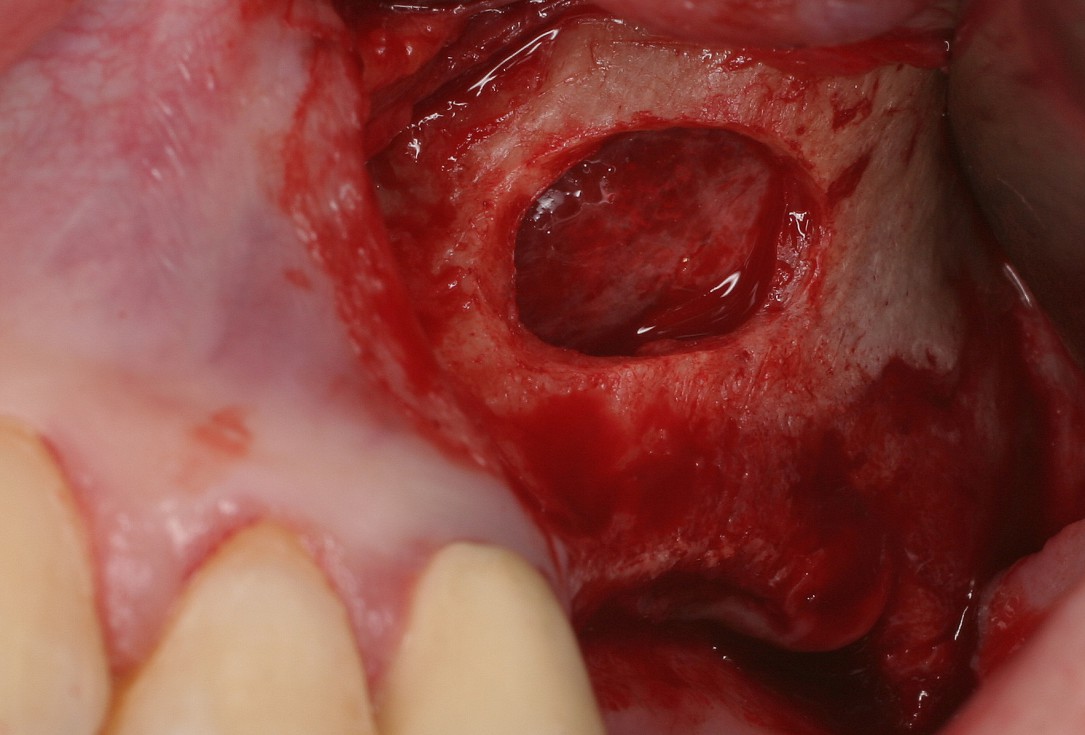
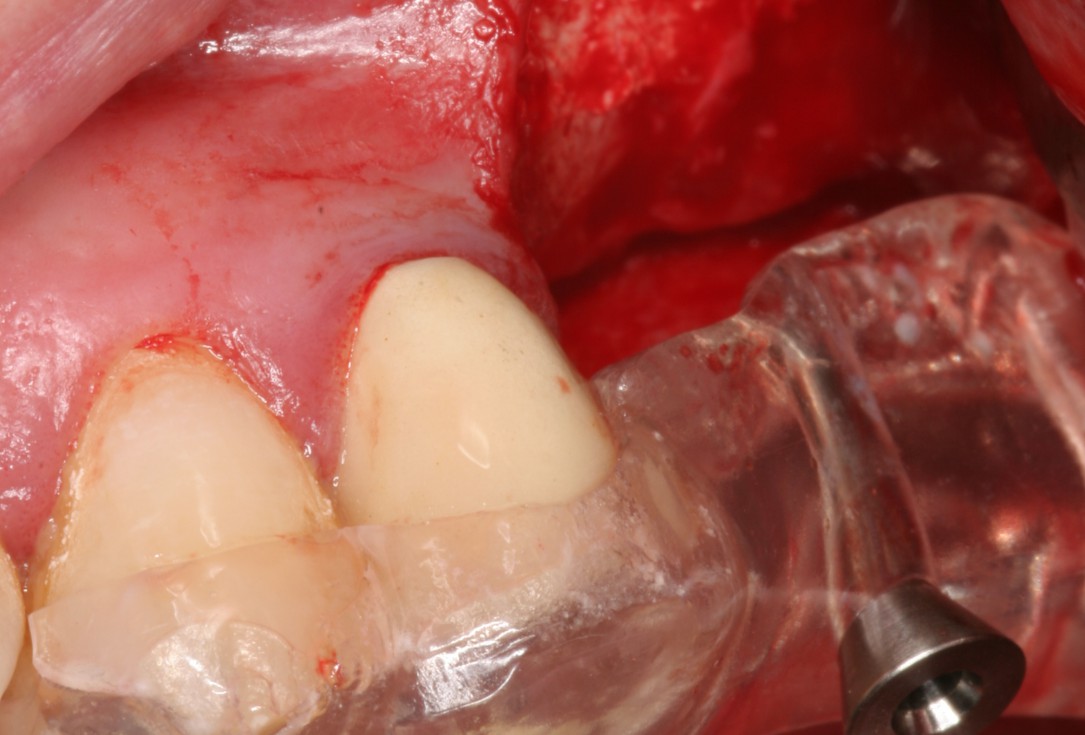
7/19 - Preparation of a lateral sinus windowSinus lift two-stage with cerabone® and Jason® membrane - Prof. Dr. Dr. D. Rothamel
-
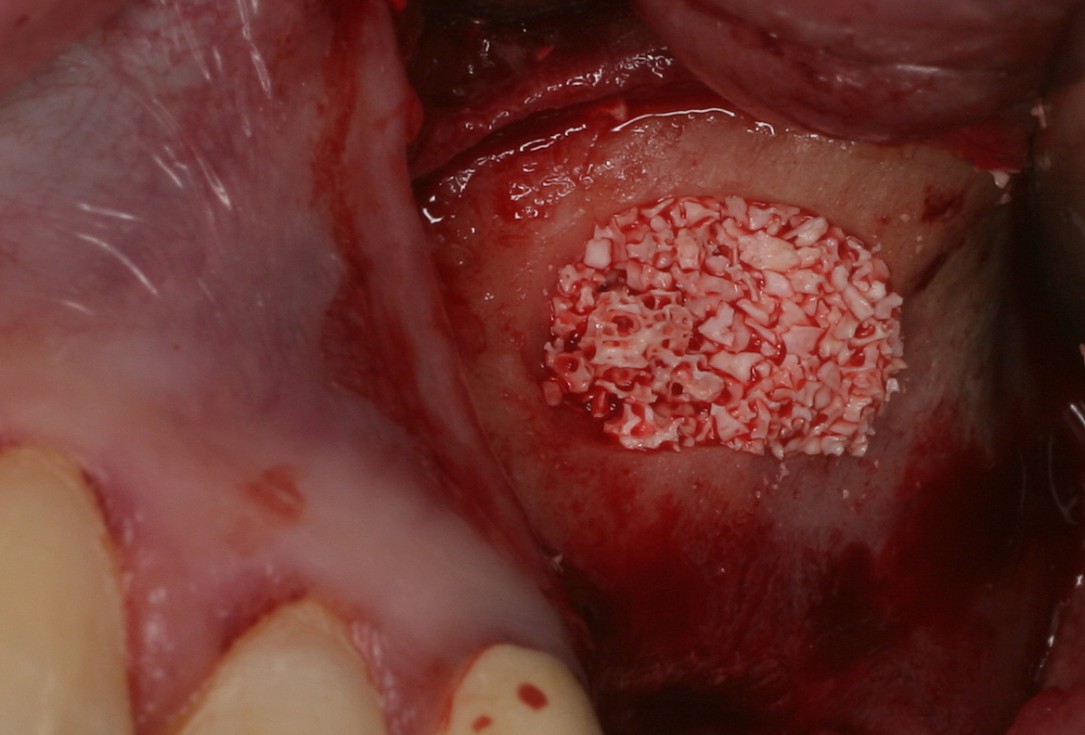
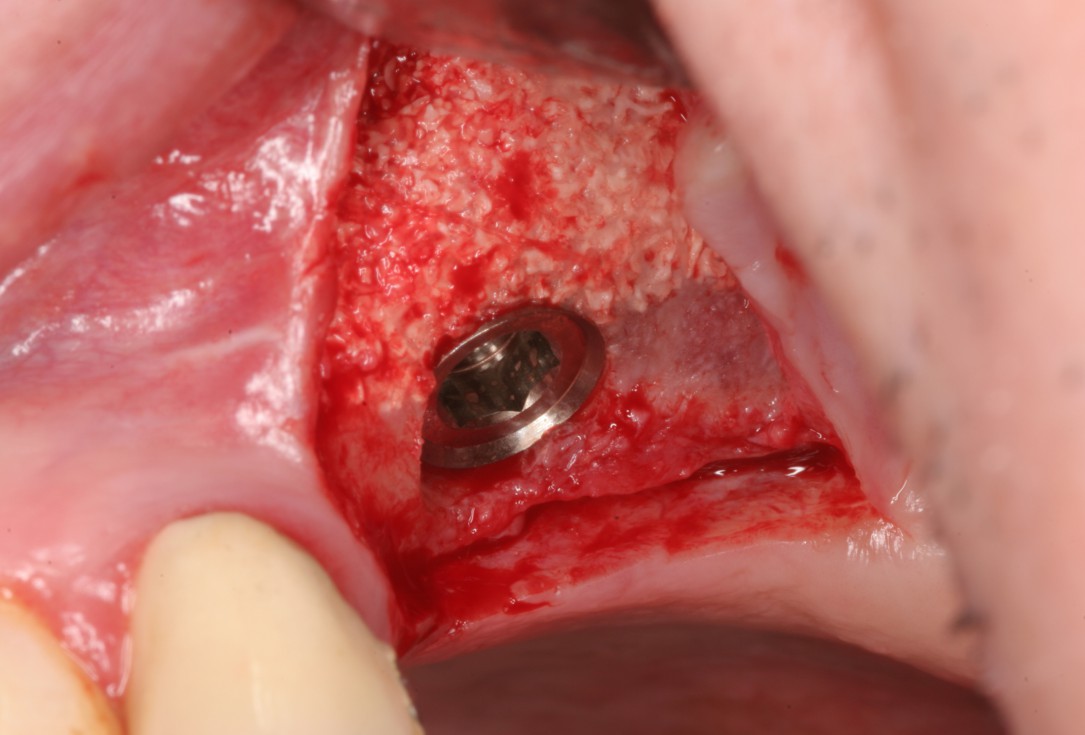
8/19 - Filling of the sinus cavity with cerabone®Sinus lift two-stage with cerabone® and Jason® membrane - Prof. Dr. Dr. D. Rothamel
-
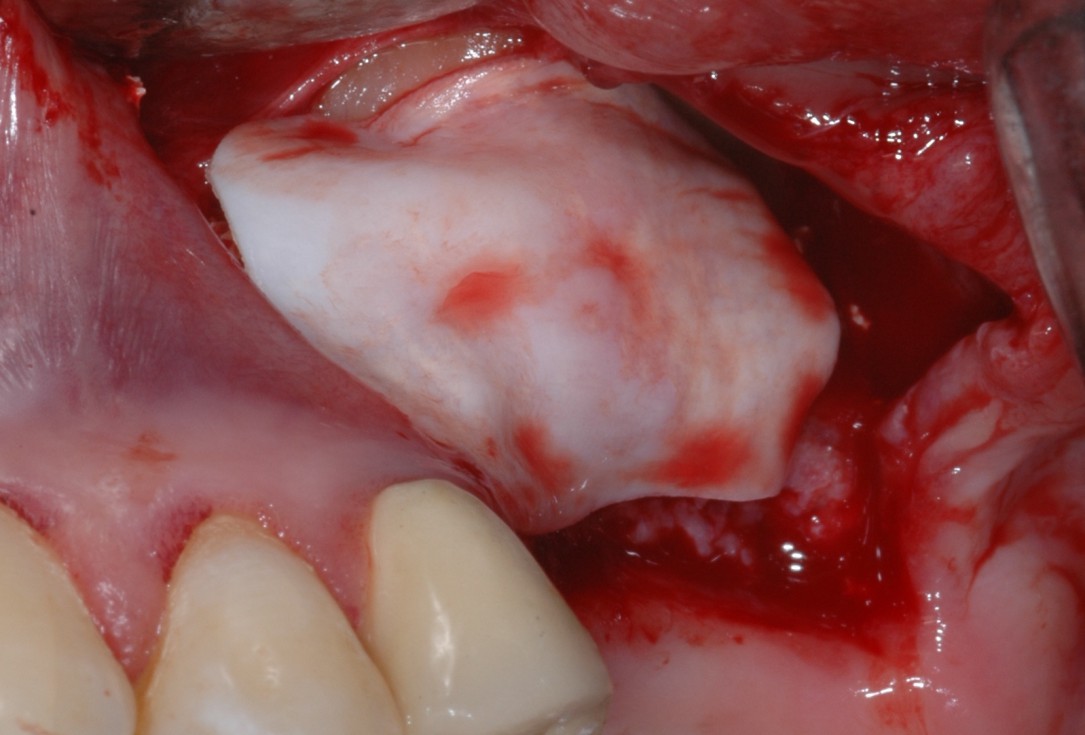
9/19 - Additional lateral augmentation with cerabone®Sinus lift two-stage with cerabone® and Jason® membrane - Prof. Dr. Dr. D. Rothamel
-
10/19 - Covering of the augmentation side with the slowly resorbing Jason® membraneSinus lift two-stage with cerabone® and Jason® membrane - Prof. Dr. Dr. D. Rothamel
-
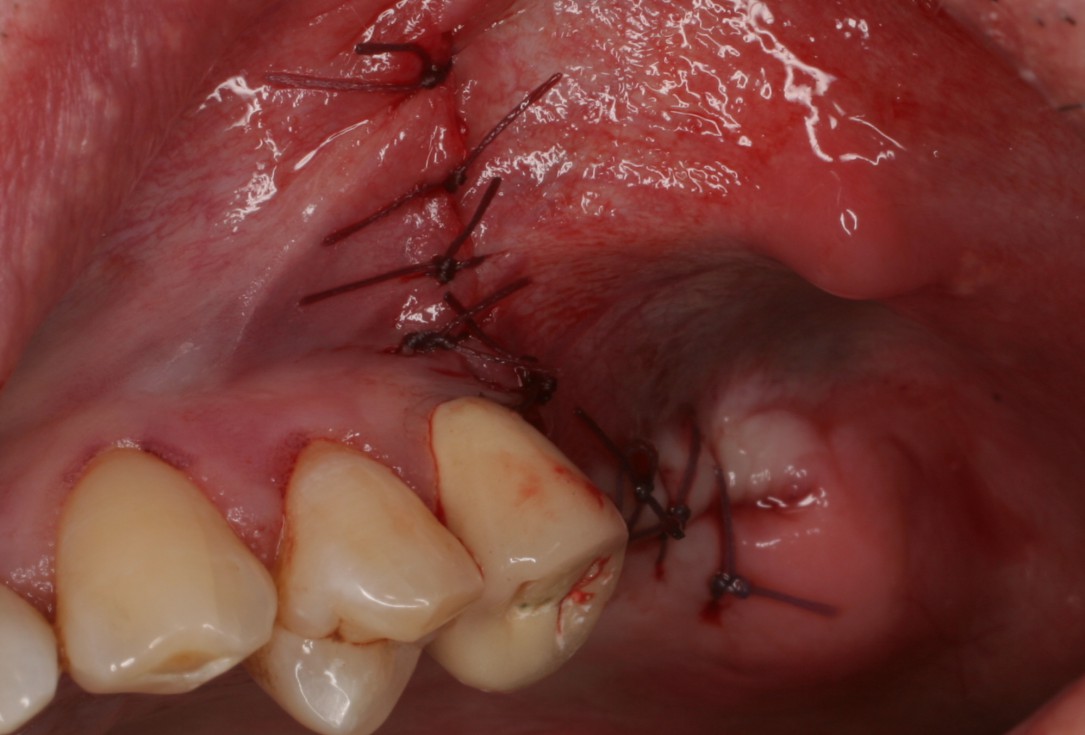
11/19 - Tension-free wound closureSinus lift two-stage with cerabone® and Jason® membrane - Prof. Dr. Dr. D. Rothamel
-
12/19 - OPG 6 months post-OPSinus lift two-stage with cerabone® and Jason® membrane - Prof. Dr. Dr. D. Rothamel
-
13/19 - Detail of OPG showing radiopacity of cerabone®Sinus lift two-stage with cerabone® and Jason® membrane - Prof. Dr. Dr. D. Rothamel
-
14/19 - Soft tissue situation at time point of re-entrySinus lift two-stage with cerabone® and Jason® membrane - Prof. Dr. Dr. D. Rothamel
-
15/19 - Very good integration of cerabone® particles without soft tissue encapsulationSinus lift two-stage with cerabone® and Jason® membrane - Prof. Dr. Dr. D. Rothamel
-
16/19 - Implant insertion with the help of a drilling templateSinus lift two-stage with cerabone® and Jason® membrane - Prof. Dr. Dr. D. Rothamel
-
17/19 - Implant placed in sufficient bone matrixSinus lift two-stage with cerabone® and Jason® membrane - Prof. Dr. Dr. D. Rothamel
-
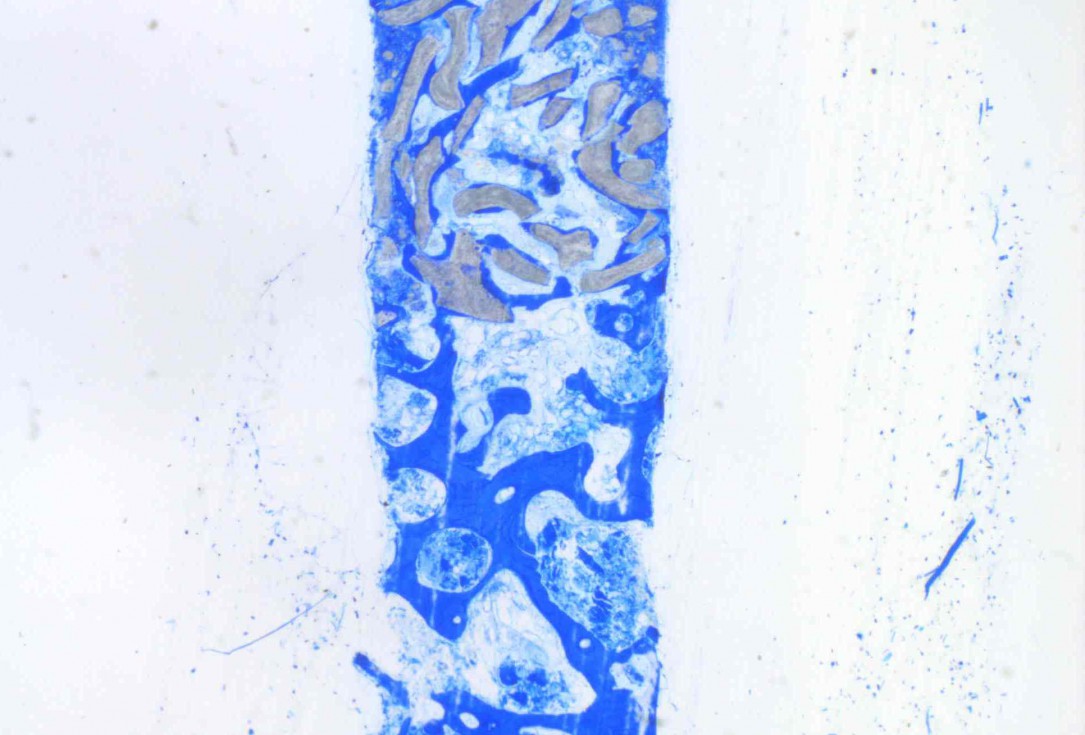
18/19 - Trephine biopsy taken at implant insertionSinus lift two-stage with cerabone® and Jason® membrane - Prof. Dr. Dr. D. Rothamel
-
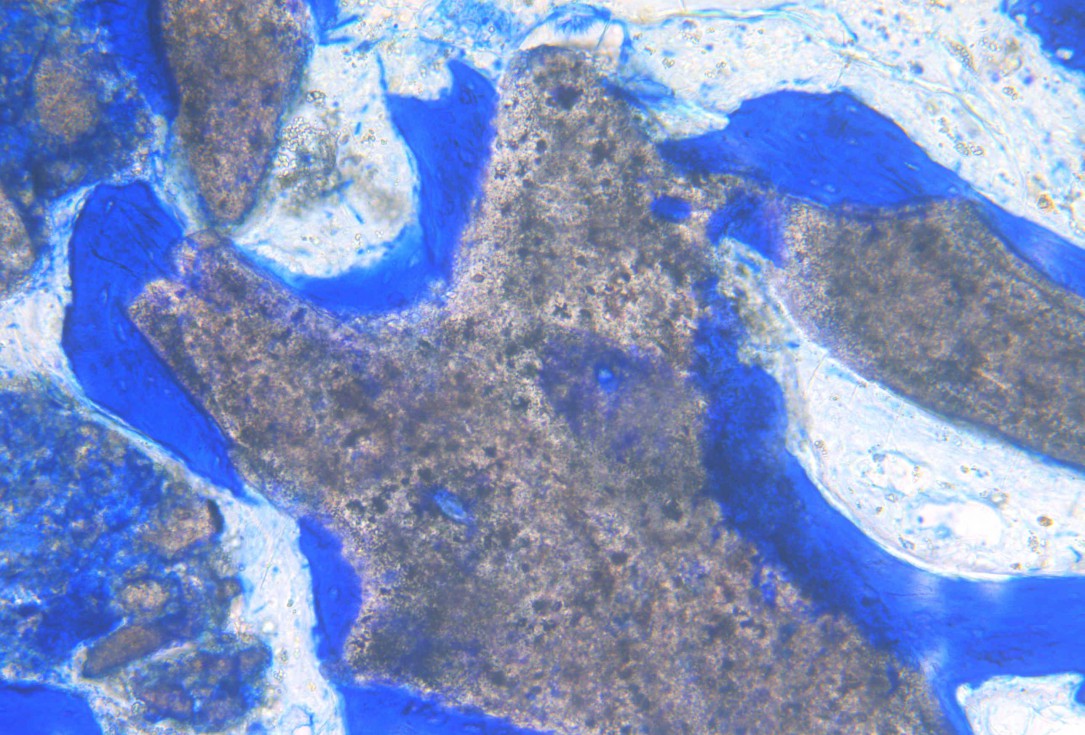
19/19 - Detail of the histology showing cerabone® particles covered by newly formed bone matrixSinus lift two-stage with cerabone® and Jason® membrane - Prof. Dr. Dr. D. Rothamel

Preoperative Ortopantomogram of the teeth planned for extraction

DVT image demonstrating horizontal and vertical amount of bone available

Extraction of tooth 21 after endodontic treatment

Implant insertion in atrophic alveolar ridge

Initial clinical situation with broken bridge abutment in regio 12 and tooth 21 not worth preserving

Initial clinical situation with gum recession and labial bone loss eight weeks following tooth extraction

Situation after tooth extraction.

Initial clinical situation

Initial situation after extraction of tooth 21 after 6 months

Situation after tooth removal.

Bone defect in area 11-21 due to two lost implants (periimplantitis) after 15 years of function

Pre-operative clinical situation: severe atrophy of the maxillary bone

60-year-old female patient presented with a chronic infection on tooth #11.
Since she has a high lip line matching the gingival margins of the adjacent central incisor and creating a root eminence is extremely important. For these reasons, the treatment of choice was an allograft bone ring enabling immediate placement of the dental implant with simultaneous regeneration of her ridge.

Initial clinical situation: 9 mm pocket depth associated with root fracture

Initial presentation of failing post retained crown with previous history of failed apicectomies and amalgam tattooing and scar tissue

Initial clinical situation with pronounced vertical and horizontal bone defect

Clinical view 8 weeks after extraction of teeth 25 and 26

Pre-operative: loss of interdental papilla between 12 and 11 associated with gingival inflammation and pus

Preoperative x-ray, multiple residual cysts of the upper jaw

Clinical situation at baseline: Situation after tooth extraction UR1 due to a failed endodontic treatment 3 months previously

Situation before extraction of the teeth

Atrophic alveolar ridge in the left mandible

Instable bridge situation with abscess formation at tooth #15 after apicoectomy

Preoperative clinical situation

Pre-operative radiographic view.

Initial situation pre-op: Central incisors with mobility 3

Initial clinical situation.

Initial situation: X-ray scan reveals eggshell thin sinus floor (1-3 mm) on both sites of the maxilla; green areas indicate the planned maxgraft® bonerings and red areas the planned implants

Pre-surgical situation. Teeth 26 and 27 missing.

Pre-op picture of affected teeth 11 and 21

Preoperative radiological situation

Clinical view of the case.

Preoperative situation – Maxillary defect in area 14-16 (loss of implant 16 due to periimplantitis, tooth 14 extracted recently and area 15 already edentulous for a while)

Initial x-ray showing bone loss around implants placed 5 years ago in another dental clinic

Initial clinical situation

Initial situation - endodontically failing tooth 22, very thin biotype, high lip line and esthetic expectations

Loss of teeth in anterior maxilla caused by periodontitis

Initial situation after root channel treatment

Preoperative CBCT analysis

Preparation of a single tooth defect with severely resorbed vestibular wall

Three implants placed in a narrow posterior mandible

Initial clinical situation with single tooth gap in regio 21

Clinical situation: 71-old patient with atrial fibrillation and Warfarin medication

Initial situation 57-year old female patient. X-ray scan reveals severe bone loss due to inflammation in region 13. Treatment plan was extraction of teeth 13 and 14 and augmentation after healing.

Initial clinical situation, regio #16

Model of the initial defect computed from a CBCT scan - buccal view

Clinical situation

Lateral view of the defect in the posterior right maxilla.

Initial clinical situation.

The patient presented with pathologic mobility of upper left central incisor. Radiographic examination revealed significant circumferential attachment loss with an unfavorable crown to root ratio.

Initial situation – Treatment plan: Replace the adhesive upper left central incisor bridge with a dental implant

Preoperative CBCT: vertical bone defects in the 3rd & 4th quadrant

Initial clinical situation: Free end situation in quadrant three and four

Initial x-ray, tooth 25 compromised and to be extracted

Preoperative x-ray, severe bone atrophy

The patient presented with severe pain in the lateral incisor and a deficient adhesive provisional. Bruxism resulted in canine loss and premature contact in the lateral incisor.

Initial x-ray, ten years post implantationem alio loco, large peri-implant bone loss