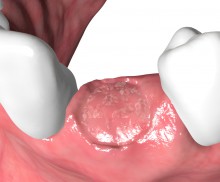
Ridge preservation with dPTFE membrane
|

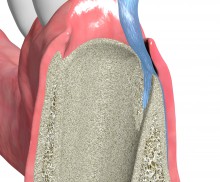
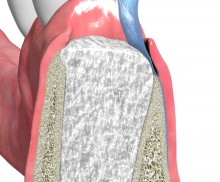
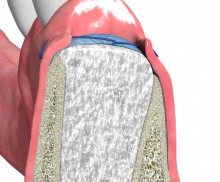
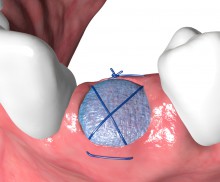
Due to its dense structure permamem® acts as an efficient barrier against bacterial and cellular penetration, and may therefore be left in place for open healing in socket or ridge preservation. In ridge preservation the membrane is placed to fully cover the socket and the deficient bone walls, and is stabilized by sutures or pins. After the healing time, permamem® can easily be removed with a pair of tweezers in a non-surgical way. The non-surgical removal of the membrane after the healing time omits the need for big surgical incisions (vertical releasing incisions), thus improving aesthetics and patient comfort. After removal, the primary healing process and the reepithelialization of the regenerating soft tissue will be completed within one month.
In order to promote the osseous regeneration, the socket should be filled with an osteoconductive bone grafting material that acts as a space holder and scaffold for precursor cells; these can then migrate into the socket and defect and mature into osteoblasts, thus triggering the construction of new bone matrix. To achieve this, a mixture of cerabone® and maxgraft® is an excellent option. While the bovine bone ensures a long-term volume stability of the grafted site, the allogenic granules consisting of mineralized collagen promote a fast integration and remodeling, thus supporting the formation of strong, vital bone. As an alternative, cerabone® or the synthetic maxresorb® granules may also be applied individually, particularly if an extended healing time of at least 5–6 months is anticipated.